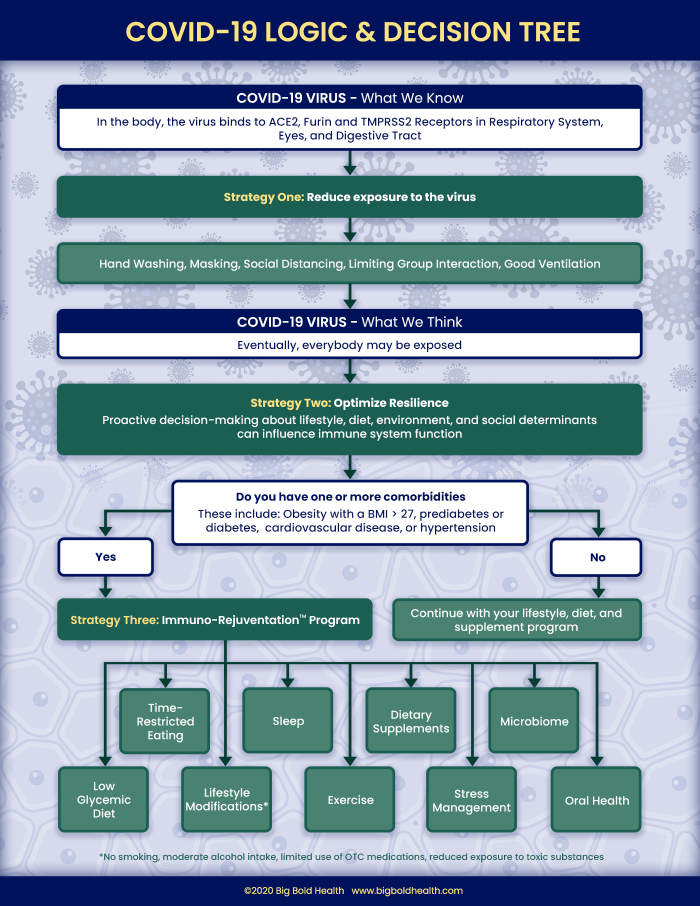
西方功能醫學教父傑佛瑞.布蘭德博士幾天前針對美國政府和大眾應該用怎樣的對策因應冠狀病毒提出客觀實際的建議,發文在Medium 雜誌。本文是重點摘譯,點擊上面照片可以讀英文全文。文中多處提到台灣防疫成功的做法,佐證為何提早防疫措施是很有效的也很必要的方法。本文最後面有一張布蘭德博士畫出的策略路線圖,邏輯簡單易懂,沒時間閱讀全文的朋友可以直接滑到最下面看那張圖,或是讀我下面兩條懶人包訊息。This is a great article just published by Jeff Bland, PhD, the highly respected “Father of western Functional Medicine”. What I am sharing here are highlights with translation into Chinese. Click on the photo above to read the entire article in English. At the end of the article is a strategy roadmap by Dr. Bland. It’s clear in logic and easy to follow.
懶人包訊息:
- 遠離病毒:口罩戴起來,適度隔離還是要做。
- 讓病毒對你沒輒 (即使已入侵你身體):用功能醫學的方法優化你的免疫系統 (也就是遠離肥胖、糖尿病、高血壓等新陳代謝疾病);到底是什麼方法?其實就是改變飲食和生活習慣(說起來容易做起來難)。
Here are the highlights. 摘譯開始…
Taiwan used past experience to their advantage when the threat of COVID-19 emerged. For context, the island of Taiwan is situated less than 100 miles from China. More than one million Taiwanese citizens work in China and routinely travel between the two countries. In 2003, many lessons were learned as a result of the SARS epidemic, and Taiwan took steps to prepare for a future viral outbreak. As concerns about COVID-19 ramped up in the early days of 2020, the leadership of this country, including President Tsai Ing-wen (the first female president of an Asian country) and Vice President Dr. Chen Chien-jen (a Johns Hopkins University-trained epidemiologist and virologist), implemented standards designed to safeguard their country from this viral threat. It is believed that the early application of testing, contact tracing, isolation, and masks, as well as the use of electronic health record data resulted not only in low infection rates, but also minimal impact on daily life and the Taiwanese economy.
年初COVID-19威脅剛出現時,台灣利用過去的經驗來發揮優勢。先來看一下台灣的背景因素,台灣島距離中國不到100英里。超過一百萬的台灣公民在中國工作,並經常往返於兩國之間。 2003年,由於SARS流行,台灣吸取了很多教訓,台灣也採取了措施,為未來的病毒爆發做準備。隨著對COVID-19的擔憂在2020年初激增,該國的領導人包括蔡英文總統(亞洲國家的第一位女總統)和副總統陳建仁(約翰·霍普金斯大學訓練出來的流行病學家和病毒學家)實施了旨在保護其國家免受這種病毒威脅的標準。後來證明,早期應用測試、接觸者追踪、隔離和屏蔽以及使用電子病歷數據不僅導致感染率低,而且對日常生活和台灣經濟的影響也最小。
On a per capita basis, the United States has experienced approximately 1200 times as many COVID-19 deaths as Taiwan. It’s a stunning contrast.
按人均計算,美國的COVID-19死亡人數約為台灣的1200倍。這是一個驚人的對比。
Preparedness has proven to be a successful strategy for flattening of the curve of disease spread and allowing society to continue to function. Taiwan has not experienced the catastrophic economic consequences that the United States is struggling with.
事實證明,對災害的提前準備是壓低疾病傳播曲線並使社會繼續運轉的成功策略。所以台灣沒有經歷美國正在努力應對的災難性經濟後果。
Can the actions taken by a relatively small population be scaled to have impact in a large country? … In the United States, which has not organized a national response plan, the infection rate is greater than 1000 cases per 100,000 people. Taiwan has an infection rate of just 2 cases per 100,000 people.
像這樣在相對較小人口的國家所採取的行動能否擴大到對一個大國產生影響? ……在尚未制定國家應對計劃的美國,感染率超過每十萬人中有1000例,台灣的感染率卻是每十萬人中只有2例。
Cell is a top tier and highly respected scientific journal. In July, it published an article entitled: “SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract.” More than 40 professionals are listed as contributing authors and participants in the research. It is complex work, however the summary points are quite accessible. The most vulnerable tissues for infection with the COVID-19 virus turns out to be the surfaces of the nasal passages and sinuses. Why? Because this part of the body has the greatest number of ACE2 receptors that can bind to COVID-19. With this knowledge in hand, the scientific logic becomes very clear. Using a cloth mask to cover the nose and mouth will reduce exposure of the upper respiratory tract to the virus. A mask, therefore, is a very important tool for personal protection against infection.
Cell是一本頂級且備受推崇的科學期刊。 7月,它發表了一篇題為“ SARS-CoV-2逆向遺傳學揭示了呼吸道中的可變感染梯度”的文章。 超過40名專業人士被列為研究的主要作者和參與者。 這是一項複雜的工作,但是摘要點很容易取得。 事實證明,人體內最容易感染COVID-19病毒的組織是鼻腔和鼻竇的表面。 為什麼? 因為身體的這一部分具有最多可以與COVID-19結合的ACE2受體。 掌握了這些知識,科學邏輯就變得非常清晰。 使用布口罩遮住鼻子和嘴巴可以減少上呼吸道對病毒的暴露。 因此,口罩是個人防護感染的非常重要的工具。
I asserted my belief that everyone will eventually be exposed to COVID-19. With this in mind, we have to consider two things that you have some level of control over: minimizing exposure risk and maximizing resilience potential. In your own home and social environment, you can proactively choose to use the same measures that have kept infection numbers low in places like Taiwan, Uganda, San Francisco, and Canada. That is, you should wash your hands frequently, keep your social distance, limit group interactions, ventilate your personal space, and wear a mask in public. These are all choices that are easy to make.
我一直以來在說的:我相信每個人最終都會接觸到COVID-19。 因此,我們必須好好思考我們至少還有某種程度掌控的兩件事:讓暴露風險最小化和提升身體對抗病變的堅韌性。像台灣,烏干達,舊金山和加拿大等地區的感染人數很低,您可以主動選擇使用這些地區民眾相同的措施來降低您自己的家庭和社交環境中的感染風險。 也就是說,您應該經常洗手,保持社交距離,限制小組互動,通風個人空間並在公共場所戴口罩。 這些都是很容易做到的選擇。
you need to determine if you are more vulnerable than others… Do you have one or more … conditions such as obesity, diabetes, hypertension, or cardiac disease. Other factors may also be relevant. For example, data has shown that being older, medically underserved, or socioeconomically disadvantaged is linked to a higher incidence of serious illness among infected individuals.
您必需確定自己是否比其他人更脆弱(更容易感染)……您是否患有一種或多種下列病症,例如肥胖,糖尿病,高血壓或心髒病。 其他因素也可能是相關的。 例如,數據顯示,年齡較大,醫療不足或社會經濟狀況不利的人群與感染個體中嚴重疾病的發生率有較高的相關性。
Lifestyle, diet, as well as environmental and social determinants (which include factors like poverty, crowding, stress, and unemployment) play significant roles in regulating the function of the immune system.
生活方式,飲食以及環境和社會決定因素(包括貧困,擁擠,壓力和失業等因素)在調節身體免疫系統的功能中也會有重要作用。
It is important for people with comorbidities to understand that implementing changes now could represent an extra layer of protection should a future exposure become inevitable. Many people don’t realize that the entire immune system turns itself over rapidly — millions of new cells every second, and a complete turnover every 100 days
對於合併症患者,還有一點很重要的認知是:如果遲早會暴露在病毒之下是無法避免的,那現在就採取應變措施可能就會有額外的保護作用。 很多人不知道的一個關於免疫系統的事實:人體整個免疫系統會快速地自我轉換 : 每秒會長出數百萬個新細胞,每100天一個人的整個免疫系統就可以完全更新(小編註:如果你有及時在飲食和生活方式上採取正確的改變)。
improving nutrition through dietary modifications is emerging as a key objective in lowering the negative effect of comorbidities on risk and severity of the infection. Francis Collins, MD, PhD has been the Director of the National Institutes of Health since 2009. He recently published an important article in JAMA with his colleague Griffin Rodgers, MD called: “Precision Nutrition — the Answer to ‘What to Eat to Stay Healthy.’” Significantly, Dr. Collins and Dr. Rodgers state the following:“Exploring how diet and nutritional status modify immune response could help explain some of the variability in COVID-19 morbidity and mortality, even in individuals without diet-related chronic disease.”
通過飲食調整來改善營養已漸漸成為降低感染風險和發病嚴重程度的主要目標。 弗朗西斯·柯林斯(Francis Collins)博士自2009年以來一直擔任美國國立衛生研究院(National Institutes of Health)主任。他最近與同事格里芬·羅傑斯(Griffin Rodgers)博士在《美國醫學會雜誌》(JAMA)上發表了一篇重要文章,題為:“精準營養 – 吃什麼才能保持健康的答案 ”。很重要的一點是,Collins博士和Rodgers博士指出:“探索飲食和營養狀況如何改變免疫反應可以幫助解釋COVID-19發病率和死亡率(在不同人之間)的某些變異性,即使在沒有與飲食相關的慢性疾病的個體中也是如此。 。”
We now understand that body fat is a key part of the immune system. There is a strong connection between excessive body fat and infiltration of that fat with activated immune cells that are in a proinflammatory state. This situation is a result of changes in the overall function of the immune system. Researchers have taken note that there is a high prevalence of obesity in countries with a high percentage of severe COVID-19 cases.
現在我們已知道,人體內的脂肪是免疫系統裡很重要的一部分。 體內多餘的脂肪 與 ”處於促炎狀態的活化免疫細胞“ 可以穿透該脂肪的程度之間存在密切的聯繫 (小編說明:也就是太多的脂肪會阻礙免疫細胞通過,因而降低了免疫細胞應該發揮的功能)。 這種情況是免疫系統整體功能變化的結果。 研究人員注意到,在COVID-19嚴重病例百分比較高的國家中,民眾的肥胖率也偏高。
In May of this year, Randy Q. Cron, MD, PhD published an article in Lancet with a provocative title: “Coronavirus is the Trigger, but the Immune Response is Deadly.” When obesity is coupled with exposure to the virus, the result can be a fatal alliance. Here’s why: chronic inflammation results from damaging alterations in the immune system. These same alterations are associated with obesity. If the controls of the immune system are disabled because of associations related to comorbidities, an individual is not only at greater risk for COVID-19 infection, but also for what has been called a “cytokine storm,” which essentially describes an overwhelming state of inflammation. In the most serious cases of COVID-19 infection, an individual does not die as a direct result of the virus, but rather from the collateral damage that takes place in the body.
今年5月,醫學博士Randy Q. Cron在柳葉刀上發表了一篇標題聳動的文章:“冠狀病毒只是觸發因素,人體的免疫反應才是致命元兇。” 肥胖加上接觸病毒會導致一個致命的結盟,原因如下:慢性發炎是由免疫系統遭到破壞導致的。 這些破壞與肥胖有關。 如果由於合併症相關的因素導致免疫系統的控制功能失效,那麼這個人不僅會面臨更高的COVID-19感染風險,也會面臨所謂的“細胞因子風暴”(cytokine storm),那是人體慢性發炎最嚴重的狀態。 在最嚴重的COVID-19感染病例中,一個人並不是直接由於該病毒而死亡,而是由於體內(免疫系統造成)的附帶損害(collateral damage )而死亡。
Your goal should not be to activate the immune system, but rather to support its proper balance and control. I have coined the term “immuno-rejuvenation” to describe this concept. … Personalizing your diet and undertaking evidence-based lifestyle interventions are the first steps in restoring immune system regulation.
您的目標不應該是“提升免疫力”,而是要維持免疫系統適當的平衡狀態和控制。 我創造了“免疫重啟再造”一詞來描述這個概念。 …個人化飲食改善 和 採取可以用結果來證明的生活方式調整 是恢復免疫系統調節的第一步。